Randomization enables unbiased estimation of treatment effects; randomization attempts to assure that treatment-groups are balanced with respect to the important covariates. Unfortunately for us shoulder surgeons, surgical treatments are rarely assigned randomly.
Propensity matching is an attempt to use observational data to compare two treatment groups by accounting for the covariates that are associated with the outcome.
The possibility of bias arises because a difference in the outcome between treatment groups may be caused by factors that predict which treatment the patient receives rather than the effectiveness of each treatment. For example if an observational study matching patients for age and sex alone retrospectively compared the recurrence rates after Bankart repair and after the Latarjet procedure, it would be at risk for an incorrect conclusion because it did not match for the size of the glenoid defect which may have affected the choice of treatment.
However, the title itself gives pause: why should a smaller operation (hemiarthroplasty) have a higher short term postoperative complication rate than a more involved procedure (total shoulder arthroplasty)? Sounds like a fundamental attribution error.
Let's take a deeper dive. The authors searched the American College of Surgeons National Surgical Quality Improvement Program database for records of patients who underwent either TSA or HA for glenohumeral osteoarthritis of the glenohumeral joint.
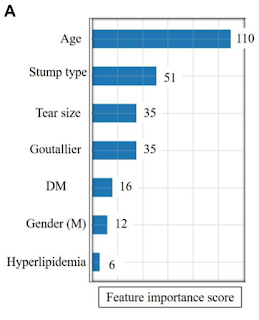
Patients in each group underwent a 1:1 propensity match for age, sex, BMI, ASA classification, diabetes mellitus, hypertension requiring medication, congestive heart failure, chronic obstructive pulmonary disease, inpatient/outpatient status, smoking status, and bleeding disorders. 2188 received TSA and 2188 received HA. The question is, "among these supposedly similar patients, what determined whether they wound up getting HA or TSA? We'll get back to that question shortly.
The HA patients had a higher rate of any adverse event (7.18% vs 4.8%), death (0.69% vs 0.1%), sepsis (0.46% vs 0.1%), postoperative transfusion (4.62% vs 2.2%), postoperative intubation (0.5% vs 0.1%), and extended length of stay (23.77% vs 13.1%).
Comment: While these differences are striking, it is apparent that putting in a plastic glenoid does not reduce the risk of death, sepsis, transfusion, intubation or extended length of stay.
As stated above, the possibility of bias arises because a difference in the outcome between treatment groups may be caused by factors that predict which treatment the patient receives rather than the effectiveness of each treatment. HA patients had a statistically significantly higher mortality probability (0.004±0.010 vs 0.002±0.003 and morbidity probability (0.027±0.015 vs 0.021±0.011) at baseline compared with the TSA cohort, even after propensity score matching. Surgeons may prefer to perform HA for high-risk patients and those with more complex pathology. Less experienced surgeons may elect to perform HA because of its simplicity. Surgeons may be more likely to perform HA on patients that have worse social determinants of health (Economic Stability, Education Access and Quality, Health Care Access and Quality, Neighborhood and Built Environment, and Social and Community Context), which are known to be associated with inferior outcomes.
Thus, while the authors state
"HA was found to increase the odds of developing these complications when baseline demographics were controlled",
perhaps a more accurate statement would be
"Patients for whom the surgeons chose HA were found have increased odds of developing these complications when the selected baseline demographics were controlled."